-
+91 8692846868
-
drmys79@gmail.com
-
Mon: 9:00am to 6:00pm, Fri to Sat: 10:00am - 4:00pm
Cord decompression surgery
Spine surgery plays an essential role in the traumatic spinal cord injury (SCI) treatment plan. Undergoing surgery shortly after the injury may have meaningful benefit for people with SCI, as studies link early surgical intervention to better long-term outcomes.
If you’ve been through a traumatic event, your spinal column and spinal cord may have sustained significant damage. A particular region or level of your spine could be unstable, and different anatomical structures (eg, vertebral bone, disc, ligament) may be compressing on your spinal cord.

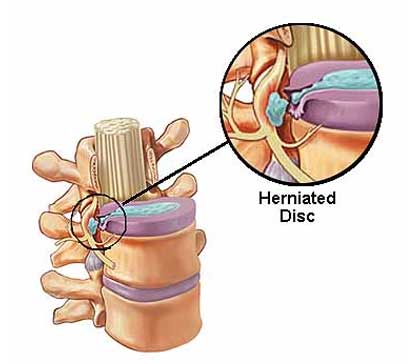
Acute and chronic disc prolapse
The bones (vertebrae) that form the spine in the back are cushioned by discs. These discs are round, like small pillows, with a tough, outer layer (annulus) that surrounds the nucleus. Located between each of the vertebra in the spinal column, discs act as shock absorbers for the spinal bones.
A herniated disc (also called bulged, slipped or ruptured) is a fragment of the disc nucleus that is pushed out of the annulus, into the spinal canal through a tear or rupture in the annulus. Discs that become herniated usually are in an early stage of degeneration. The spinal canal has limited space, which is inadequate for the spinal nerve and the displaced herniated disc fragment. Due to this displacement, the disc presses on spinal nerves, often producing pain, which may be severe.
Decompression surgery for lumbar and cervical canal stenosis
Cervical spinal stenosis is a bone disease involving the narrowing of the spinal canal at the level of the neck. It is frequently due to chronic degeneration, but may also be congenital. Treatment is frequently surgical.
Cervical spinal stenosis is one of the most common forms of spinal stenosis, along with lumbar spinal stenosis (which occurs at the level of the lower back instead of in the neck). Thoracic spinal stenosis, at the level of the mid-back, is much less common. Cervical spinal stenosis can be far more dangerous by compressing the spinal cord. Cervical canal stenosis may lead to serious symptoms such as major body weakness and paralysis.

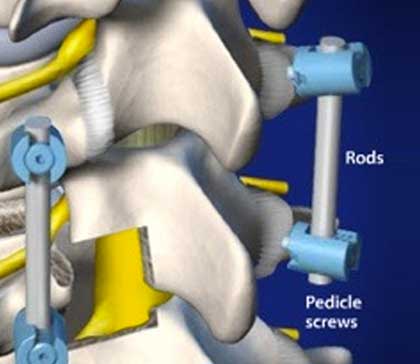
Posterior lumbar inter body fusion PLIF
Instrumented posterior lumbar interbody fusion (iPLIF) is a common spinal fusion surgical technique for addressing low back pain resulting from degenerative lumbar spine disorders. It involves fusion of two or more levels utilizing screws, rods, and an interbody graft.
It has a theoretical advantage over instrumented posterolateral fusion (iPLF) in that it provides better support for the vertebra along with several potential neurological benefits, but as of 2011 evidence demonstrating actual improved clinical outcomes was lacking.

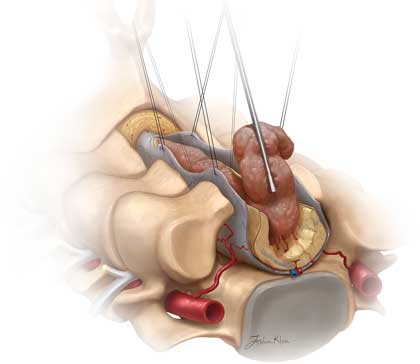
Total lumbar interbody fusion TLIF
TLIF surgery, or transforaminal lumbar interbody fusion, is an approach to spinal fusion surgery in which the neurosurgeon accesses the lower spine through the intervertebral foramen. The intervertebral foramen is the opening between the bones of the spine, called vertebrae, through which nerves leave the spinal cord and en route to other parts of the body.
TLIF is one of several different approaches to spinal fusion surgery. Spinal fusion is performed to join together two or more spinal vertebrae, eliminating movement between them. This is done by removing the intervertebral disc between the two vertebrae, which normally enables the spine to bend and rotate, and inserting a bone graft in its place. The bone graft heals over several months, fusing the vertebrae together and stabilizing the spine.
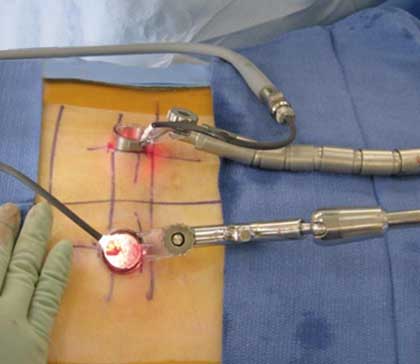
Minimally invasive spine surgery
Minimally invasive spine surgery (MISS) is a type of surgery on the bones of your spine (backbone). This type of surgery uses smaller incisions than standard surgery. This often causes less harm to nearby muscles and other tissues. It can lead to less pain and faster recovery after surgery.
The standard method of spine surgery is called open surgery. This uses a long incision down the back. The muscles and soft tissue around the spine would need to be moved away. In some cases, tissue would need to be removed.
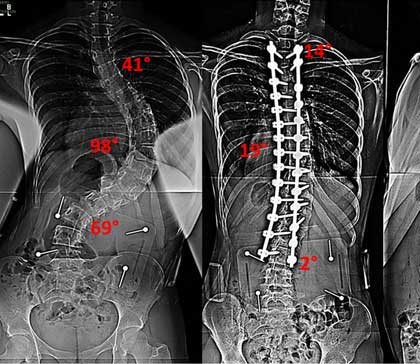
Paediatric spine surgery – scoliosis
Minimally invasive scoliosis surgery is a type of procedure done to fix an abnormal curve of the spine known as scoliosis. This type of surgery uses smaller incisions than open surgery.
The spine has some normal curves forward and backward. But it should not curve to the side. With scoliosis, the spine curves to the side in an S-shape or a C-shape. If the curve is severe, it can cause uneven shoulders or a body that appears to tilt to one side.
excision of spinal tumours
Not all spinal tumors require immediate surgical treatment. Sometimes the tumor is observed over time for change. This is a common approach in small benign (non-cancerous) tumors. Larger benign tumors, certain types of spine cancer (malignant), and progressive tumors may require surgical intervention.
Spine surgery may be recommended to remove a benign or malignant tumor, reduce its size, and/or relieve persistent back or neck pain, balance problems, difficulty walking, and bowel or bladder dysfunction.
Anterior and posterior decompression and fixation in Potts spine
Pott disease is tuberculosis of the spine, usually due to haematogenous spread from other sites, often the lungs. The lower thoracic and upper lumbar vertebrae areas of the spine are most often affected.
It causes a kind of tuberculous arthritis of the intervertebral joints. The infection can spread from two adjacent vertebrae into the adjoining intervertebral disc space. If only one vertebra is affected, the disc is normal, but if two are involved, the disc, which is avascular, cannot receive nutrients, and collapses. In a process called caseous necrosis, the disc tissue dies, leading to vertebral narrowing and eventually to vertebral collapse and spinal damage. A dry soft-tissue mass often forms and superinfection is rare.